LUSAKA – Minister of Health, Dr. Elijah Muchima, has emphasized the vital role that Community-Based Volunteers (CBVs) play in Zambia’s healthcare system, describing them as the backbone that connects health facilities to the people who need them most.
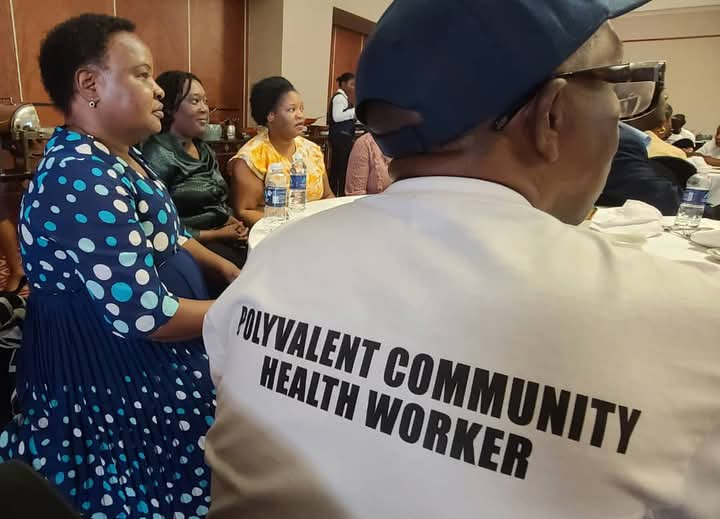
Dr. Muchima’s remarks were delivered on his behalf by the Permanent Secretary for Technical Services, Dr. Kennedy Lishimpi, during a media and stakeholder engagement meeting highlighting the role of Polyvalent Community-Based Volunteers (PCBVs).
He stated that CBVs serve as first responders, educators, and advocates, ensuring that even the most vulnerable populations have access to essential health services. He further explained that PCBVs represent a specialized group of CBVs trained across multiple thematic areas to deliver comprehensive, community-centered health services in both rural and urban communities.
“The Integrated Community Health Services Package Training, which spans three weeks, equips PCBVs with the necessary knowledge and skills to empower communities in taking charge of their health,” Dr. Muchima said.
He noted that this training enables PCBVs to provide critical healthcare services, ranging from health promotion to disease prevention, thereby alleviating pressure on Zambia’s already stretched health facilities. However, he stressed the need for greater investment in these volunteers by providing them with the right tools and resources to enhance their efficiency and improve health outcomes across communities.
Meanwhile, UNICEF Representative Dr. Nejmudin Kedir Bilal underscored the importance of strengthening the community health workforce, stating that community-based workers play a pivotal role in delivering cost-effective healthcare, particularly in hard-to-reach areas.
“Community health workers, as social agents of change, also need the support of the media to enhance access to life-saving services,” Dr. Bilal noted.
He reiterated UNICEF’s commitment to strengthening community-based healthcare systems in Zambia in collaboration with the Ministry of Health.
A Polyvalent CBV is a multi-skilled community health volunteer trained to perform a broad range of tasks, including preventive, promotive, and curative health activities within communities.
Ministry of Health Communications and Public Relations Unit Zambia






OTHER ARTICLES
Editorial — Prevent, inform, and act for women’s health in Africa
Kenya : Government Prioritises Maternal Health and Strengthens Support for Community Health Promoters
Strengthening pandemic prevention, preparedness, and response capacities in Senegal using the “One Health” approach